Tenured faculty position
The Department of Biology at Indiana University Indianapolis invites applications for a tenured faculty position at the rank of Associate or Full Professor to begin March 1, 2025. Applicants must have a successful research program in the study of Hydrocephalus.
Research
The founding members of the Hydrocephalus Research Center are all colleagues and collaborators on two Department of Defense grants supporting preclinical studies targeted to developing drug treatments using genetic and induced (post-hemorrhagic and post-traumatic) forms of hydrocephalus in rodents and in a pig model of post-hemorrhagic hydrocephalus.
To date, the potential treatments target CSF production, neuroinflammation and neuronal cell protection. The proposed experiments will also explore co-therapy of agents targeting multiple aspects of hydrocephalic development and associated sequelae such as changes in cognition, vision, pain and gait disturbances.
Hydrocephalus is a devasting disease for which there are no pharmaceutical treatments.
Currently the standard of care involves brain surgery—most usually the placement of a shunt to drain excess cerebrospinal fluid (CSF) from the brain to another area of the body. However, shunts routinely fail for a variety of reasons including infection, blockage and equipment malfunction predisposing the patient to multiple brain surgeries.
While pediatric hydrocephalus is perhaps the most recognizable form, there are multiple causes of this condition in older children and adults including traumatic brain injury, stroke, infection and genetic predisposition. Regardless of the precipitating factors, there is an excess of CSF in the brain and an enlargement of the cerebral ventricles.
It is our hypothesis that pharmaceuticals that could decrease CSF production on an as-needed basis would be helpful in treating most forms of hydrocephalus. Alternatively, pharmaceuticals that target aspects of the pathological changes such as inflammation and neuronal cell death would also be beneficial. Rational drug design for such potential treatments is based on a more detailed understanding of the production of CSF by the choroid plexus epithelium as well as the pathological changes that occur in response to the precipitating causes. The small tissue comprising the choroid plexus produces approximately 500 ml of CSF per day, the composition of which varies according to physiological, diurnal, and pathophysiological influences. The pathological changes likely include production of toxic intermediates, inflammation, changes in fluid electrolyte homeostasis, and ultimately, cell damage and death.
Description of the video:
Hydrocephalus is a build up of the cerebral spinal fluid inside of the brain. People are most familiar with it in the pediatric population, and there it is about one in a thousand most common in premature infants. But what people don't realize is that it is a similar problem in adults. Currently, the only treatment for hydrocephalus is brain surgery. Our ultimate goal is to find a drug that we can use to treat hydrocephalus. I'm Bonnie Blazer-Yost. I am a professor of biology in the School of Science here at IUPUI. And what we're studying in the brain is what are the processes that cause the production of cerebral spinal fluid? And analogous question would be, what goes wrong? And is there some step where we can intervene with a potential drug? The DOD is interested in this, as you might well imagine, because of traumatic brain injury. The active duty military, of course, are most prone to the post-traumatic form of hydrocephalus. The DOD veteran population is like all populations, aging. So the normal pressure hydrocephalus is important to them as well. In talking with our colleagues we realized that there's probably a lot of commonality. We thought it would be nice to have a center to bring all of this together. It has become a point of collaboration across campus. The neuroscience units on campus, particularly the medical school, have shown interest. We're hoping that the center is a conduit for bringing people together here in Indianapolis, because having our clinical colleagues join us is very, very powerful to have multiple views of hydrocephalus and how we might approach treatment options.
Doctoral students at IU Indianapolis lead pursuit for groundbreaking hydrocephalus drug treatments
The only treatment currently available for hydrocephalus is brain surgery, and researchers at IU Indianapolis’ Hydrocephalus Research Center are on a mission to change that.

3 science students battle frigid San Francisco waters to raise money for hydrocephalus research
After training for six months at the IU Natatorium, IU School of Science students Fatemeh Bidgoli, Verayna Newland and Cameryn Davis swam 1.8 miles from Alcatraz Island to mainland San Francisco to... Read more about 3 science students battle frigid San Francisco waters to raise money for hydrocephalus research
Swimming from Alcatraz Island to San Francisco for hydrocephalus research
September 2, 2024
Three researchers from the Hydrocephalus Research Center participated in the 2024 Alcatraz Swim with Team Hydro, a group dedicated to raising awareness about and finding a cure for hydrocephalus.

$11.7M from Department of Defense to fund research on common complication to traumatic brain injury
Researchers at the School of Science at IUPUI will lead grants to fund research toward an effective drug treatment for hydrocephalus, a condition commonly associated with complications from traumat... Read more about $11.7M from Department of Defense to fund research on common complication to traumatic brain injury


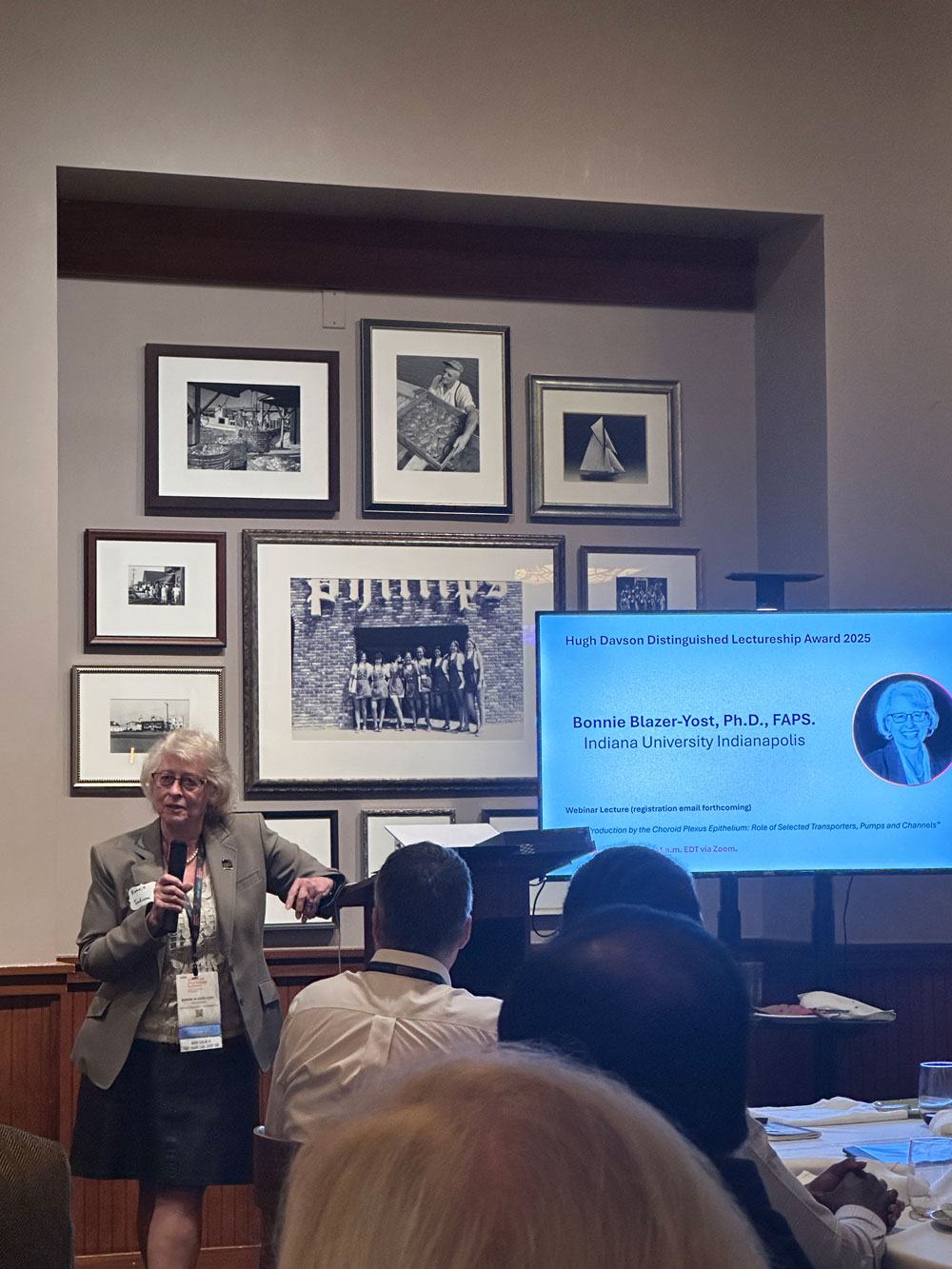
Bonnie Blazer-Yost, Ph.D.
Professor of Biology, IU Indianapolis
Director, Hydrocephalus Research Center
Prof. Blazer-Yost is a transport physiologist whose main research interest is the regulation of epithelial ion transport particularly in response to stimuli such as hormones and other effectors. Her laboratory studied polycystic kidney disease (PKD) particularly the mechanisms underlying the growth of cysts. In the PKD field, she has experience in taking a potential drug treatment (PPARg agonists) from an initial observation in cultured cell studies, through animal models and into a human clinical trial for which she was a Co-PI. Currently, the focus of this laboratory is studying the mechanisms of hydrocephalic development in a variety of preclinical models with a view to developing a drug treatment for hydrocephalus. She is the corresponding PI of two large DoD grants supporting preclinical drug development for hydrocephalus.

Lauren Jantzie, Ph.D.
Associate Professor of Pediatrics, Johns Hopkins University
Dr. Jantzie is a neuroscientist and neuropharmacologist dedicated to the pathophysiology of brain injury and its sequela. She is an expert in neural-immune communication and inflammatory signal transduction. In addition to studying neurorestoration in hydrocephalus, her lab is examining the intersection of brain and peripheral inflammation and immune activation. Together with high-resolution neuroimaging of functional and anatomical connectivity, and touchscreen cognitive assessment, she uses a sophisticated clinical biomarker detection and identification platform in her work to quantify inflammatory proteins in biological fluids and tissues.

Teri Belecky-Adams, Ph.D.
Professor of Biology, IU Indianapolis
Dr. Belecky-Adams is a vision biologist specializing in retinal health and disease. Dr. Belecky-Adams is an expert in factors that trigger astrogliosis and microgliosis in retinal disease and determining a role for inflammation in diabetic retinopathy. Her laboratory has discovered the role of a cilia protein in photoreceptor development and degeneration using the rapidly progressing Tmem67-/- rat hydrocephalus model. She is using preclinical rat models of hydrocephalus to study papilledema and vision problems associated with the disease.

Shenandoah Robinson, M.D.
Professor of Neurosurgery, Johns Hopkins University
PI of projects 1 and 3
Dr. Robinson is a pediatric neurosurgeon who cares for children and adults with hydrocephalus. She is internationally recognized as an expert in posthemorrhagic hydrocephalus and consequences of brain injury, including trauma. Dr. Robinson brings extensive expertise in development of clinically relevant brain injury models, oligodendrocyte biology and mechanism of brain injury and repair. Her research on neurorepair with erythropoietin (EPO) provided mechanistic support for the translation of EPO into clinical trials for preterm infants. Dr. Robinson is also an expert in cell culture explant biology, unbiased stereology, and behavioral testing. She is PI of a PRMRP award and an Expansion Award exploring treatment of acquired symptomatic hydrocephalus.

R. Timothy Bentley, BVSc, MRCVS
Associate Professor, Purdue University School of Veterinary Medicine
Dr. Bentley is a veterinary neurosurgeon with a specialty in intracranial surgery. He was instrumental in developing a porcine experimental model of post-hemorrhagic hydrocephalus, and subsequently performing in vivo studies to evaluate a novel ventriculo-peritoneal shunt. He also leads a brain tumor research program, using spontaneous brain tumors in pet dogs as a model of human glioblastoma. He also conducts studies on the application of MRI in the diagnosis of brain tumors and hydrocephalus.

Gregory Knipp, Ph.D.
Dr. Knipp's laboratory is dedicated to the utilization of new and improved models for assessing pharmaceutical performance. The laboratory's research interests include preclinical in vitro and in vivo ADMET screening, physicochemical characterization, early formulation development, and performing pharmacokinetic studies of new and traditional chemical entities. His laboratory has been recently focused on the development of a novel, direct contact human blood brain barrier triculture model for screening permeability-linked neuroactivity. Cultured in the presence of neurons, this flexible platform in vitro model has been applied to assess neurotoxicity and screening compounds with an observed neurotherapeutic/neurotoxic effect.

Robyn McCain, B.S., RLATg
Robyn received her B.S. in Animal Science from Oklahoma State University. She has been the manager of the Purdue Translational Pharmacology Unit since 2010. Robyn was previously employed with Bioanalytical Systems Incorporated for 12 years where she developed most of the rodent catheters and surgical procedures for the Culex Automated Blood Sampling System and the Culex-L pigturn units. She is the only user of the Pigturn/Culex-L units and has trained many of the top 10 large pharma in use of the Culex rodent units. Prior to joining BASi she worked for the University of Memphis in the Biomedical Engineering group doing work in Cardiac Electrophysiology as well as assisting researchers at St. Jude Children's hospital in areas of cancer research.

Verayna Newland
Verayna received her B.S. in Biology from Indiana University-Purdue University Indianapolis (IUPUI) in 2022. She is now a Ph.D. candidate in Dr. Blazer-Yost's lab studying ion channels on the choroid plexus epithelium.

Sarah Connors, B.S., MBA
Born and raised in Greenwood, IN, Sarah attended Purdue University where she earned her Bachelor’s in Animal Sciences then went on to attend Anderson University, earning her Master’s in Business Administration in the summer of 2022. Sarah now works as the manager of the Hydrocephalus Research Center. Her role in the lab is to review the budgets and other administrative things.

Makenna Reed, B.A.
Makenna received her degree from Central College (Pella, Iowa) in 2018. She is currently a PhD candidate in Dr. Blazer-Yost's laboratory. Her current project focuses on elucidating common mechanisms between different hydrocephalic presentations with the goal of developing drug candidates that move this research towards clinical trials.

Cameryn Davis
Cameryn is a third-year undergraduate at Indiana University-Purdue University Indianapolis. She is double majoring in Chemistry and Biology and is a current research fellow of UROP. In Dr. Blazer-Yost's laboratory, she focuses on choroid plexus epithelium ion channels using Ussing-Chamber electrophysiology.

Audrey Kruse
Audrey completed a B.S. in Neuroscience and Psychology from Indiana University-Purdue University-Indianapolis. Recently awarded with a University Fellowship, she is now pursuing a PhD in Biology under the direction of Dr. Bonnie Blazer-Yost at Indiana University Indianapolis. Currently, her research is focused on epiplexus immune cells of the choroid plexus and their role in the development of hydrocephalus and neuroinflammation across different models of the disease (genetic and induced hydrocephalus).

Fatemeh Omidi Bidgoli
Fatemeh is currently pursuing a Ph.D. in Biology at Indiana University-Purdue University Indianapolis. She completed her undergraduate studies in Biotechnology at Kharazmi University in Tehran, Iran. Her research, conducted under the mentorship of Dr. Bonnie Blazer-Yost, centers on developing novel pharmacological treatments for hydrocephalus, aiming to avoid surgical methods.
Spencer Patterson
Spencer is a third year undergraduate student majoring in neuroscience. In Dr. Belecky-Adams lab, he is currently working with and assisting Umanga Poudel with the ongoing research into the role of TAK1 in diabetic retinopathy.

Jack Reinoehl
Jack is currently pursuing a Master’s degree in Biology at Indiana University-Purdue University Indianapolis. He obtained his B.S. in Biology from the University of Cincinnati. He is currently researching the mechanisms of specific proteins and their roles in Diabetic Retinopathy in Dr. Belecky-Adams' Lab.

Nasim Shafiee Nejad
Nasim holds a Bachelor degree in Cell and Molecular Biology. She joined Dr. Belecky-Adam's lab as a Master's student in 2023. She is currently a Ph.D. student and her current research is focused on papilledema associated with hydrocephalus.

David Audu, Ph.D.
David earned his bachelor's degree in Zoology from the University of Jos in Nigeria. He pursued his master's and doctoral degrees in Zoology, specializing in Animal Physiology, at the Federal University of Agriculture in Abeokuta, Nigeria. In his postdoctoral research at Prof Bonnie's lab is to explore potential drug treatments for hydrocephalus.

Maryam Torabi
Maryam completed her B.S. in Animal Biology at Arak university in Iran and M.S. in Cellular and Molecular Biology at University of Science and Research in Iran. She is currently a PhD candidate in Dr. Blazer-Yost's laboratory. Her research focuses on the effects of cytokines in causing inflammation in hydrocephalus and studying new drug approaches to find sustainable treatment.
Hamid Aboutalebkadkhodaeian, Ph.D.
Hamid is an anatomist and recieved his Ph.D in anatomical science from Tarbiat Modares University in Iran. He also has experience as an assistant professor in medicine. Hamid's research focus was on in vitro and in vivo mechanism of retinal diseases like age-related macular degeneration (AMD), cell replacement therapy in AMD animal model. In the Indiana University, Biology department he is working on mechanisms of retinal papilledema related to hydrocephalous using animal models.

Gowthami Mahendran, Ph.D.
Gowthami earned her bachelor's degree in Molecular Biology and Biochemistry from the University of Colombo in Sri Lanka. She then pursued a Ph.D. in Biochemistry at the University of Notre Dame, Indiana where her dissertation work concentrated on multi-omics studies of Miller-Dieker Syndrome, a rare brain condition. In her postdoctoral research, she will focus on the phosphoproteomics of hydrocephalus to assist in identifying biomarkers for therapeutic development.

Scott Mitchell, MD
Scott Mitchell has studied biochemistry at Bowdoin College, biomedical engineering at Dartmouth College, medical school at University of Vermont and currently a senior neurosurgery resident at IU School of Medicine. He has research interest in hydrocephalus and is clinically pursuing pediatric and endovascular neurosurgery. He is actively involved in the development of small and large animal models of post hemorrhagic hydrocephalus with Dr. Blazer-Yost.

Yanping Zhang
Yanping Zhang received her M.S degree in laboratory technology. She now works as a research technologist in Bonnie Laboratory.
Jane Obiako, M.S.
Jane earned her bachelor's degree in human Anatomy at Ebonyi State University, Nigeria and a master's degree in human Anatomy at the University of Ibadan, Nigeria where she got exposed to Hydrocephalus research. She is now pursuing a Ph.D. in Biology at the Hydrocephalus Research Center, Indiana University Indianapolis, under the supervision of Prof. Bonnie Blazer-Yost to explore novel non-surgical therapeutic strategies for hydrocephalus treatment.

Snehvir Kaur
Sneh is an undergraduate student at IU Indianapolis, pursuing a major in neuroscience. She is actively involved in the lab, led by Dr. Bonnie Blazer-Yost, where she collaborates with Fatemeh Omidi Bidgoli to pioneer innovative pharmacological treatments for hydrocephalus, with a focus on non-surgical interventions.
Amber Zack
Amber completed her B.S. in General Science at the University of Nevada, Las Vegas. She is currently a PhD student in Dr. Belecky-Adams’ laboratory. Her research focuses on papilledema associated with hydrocephalus and disrupted circa circadian rhythms as a result of the loss of retinal ganglion cells.
Dr. Alexa Bramall
As an assistant professor of neurosurgery working in adult hydrocephalus, my research focuses on cerebrospinal fluid (CSF) pathways in the brain and the mechanisms by which hydrocephalus develops. In addition to intersecting every area of neurosurgery from pediatrics to trauma, abnormalities in CSF physiology have been implicated in a multitude of neurological diseases, from Alzheimer’s disease to depression.
My basic science research involves identifying the mechanisms of intracranial pressure regulation by choroid plexus epithelial cells. The lab uses genetic mouse models to explore important genes and/or proteins involved in CSF regulation. Our goal is to develop novel, long lasting and minimally invasive strategies to diagnose and treat CSF flow disorders.

Dr. Yun (David) Yung
Assistant Professor Yun (David) Yung earned his dual AB degrees in Molecular Cell Biology and Cognitive Sciences from the University of California, Berkeley and his Ph.D. in Biomedical Sciences from the University of California, San Diego. He subsequently continued his research at Scripps Research and Sanford Burnham Prebys Medical Discovery Institute prior to joining both The Scintillon Research Institute in San Diego and The Hydrocephalus Research Center (HRC) at Indiana University. Dr. Yung’s research in numerous fields has led to key discoveries. First, bioactive lipids released during bleeding can cause fetal and neonatal forms of hydrocephalus in children and such pathways can be preventatively or therapeutically modulated for potential non-invasive treatments for hydrocephalus. His lab currently works closely with other investigators at the HRC as part of the DoD-funded consortium to examine novel hydrocephalus models, pathways, and therapeutics. Second, the development and use of single nuclei sequencing methodologies, including isolation of cell nuclei, RNAseq, and barcoding probes, can provide sufficient information to identify cell types of the brain; this strategy can be used for many tissues in the body and is a foundational approach for numerous single cell discovery and diagnostic efforts. Third, altered genomics exist in normal brain cells and further imbalances can be linked mechanistically to neurological diseases, such as Alzheimer’s disease and Down syndrome. Finally, Professor Yung’s focus extends to translational medical studies on iPSCs and their use in the treatment of disorders such as type 1 diabetes, neuroinflammation, and generalized aging using mRNA-based directed differentiated iPSCs into specific cell types and using partial reprogramming for cellular rejuvenation.
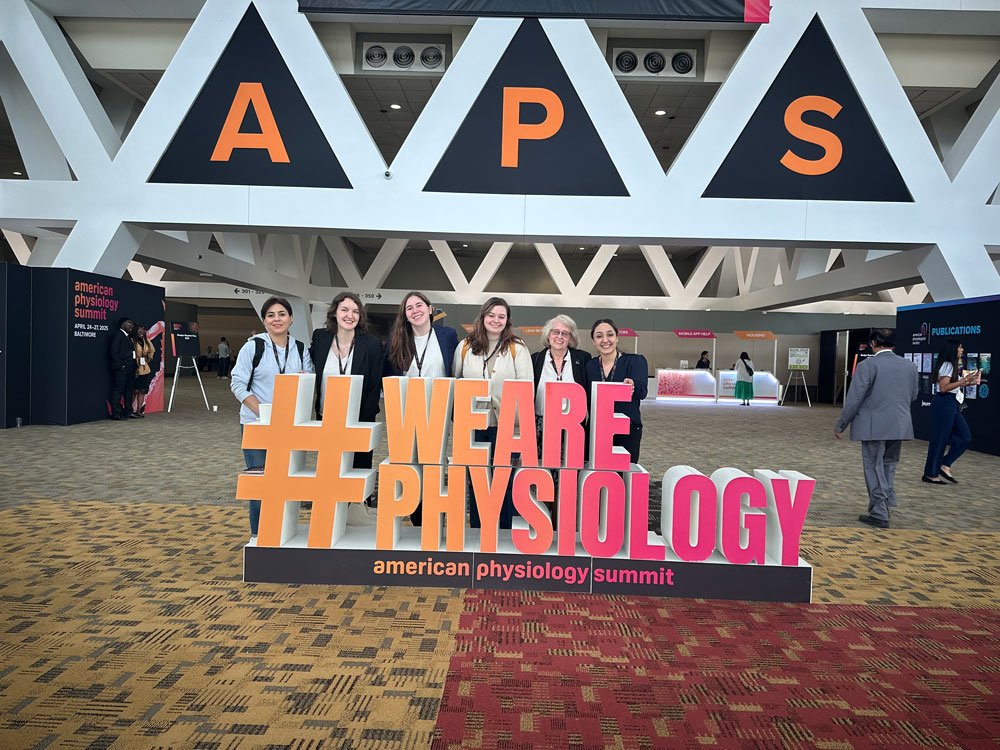
2025 American Physiological Society Conference - Baltimore, Maryland